The Connection Between Alcohol Use Disorder and Trauma

In the shadowy corners of our lives, trauma and alcohol use disorder often lurk, entwined in a sinister dance. This intricate relationship, fraught with complexities, is what we’ll delve into today.
It’s no secret that trauma can leave deep scars, invisible yet profoundly impactful. Similarly, alcohol use disorder isn’t just about the physical addiction; it’s a reflection of an inner turmoil, a desperate attempt to escape reality.
In this exploration, we’ll unravel the threads connecting these two distressing conditions. We’ll shed light on how trauma can trigger alcohol use disorder and how, in turn, this dependency can exacerbate the traumatic experience. So buckle up, as we embark on this enlightening journey into the human psyche.
Understanding Trauma and Its Effects
To begin, let’s dive into the world of trauma and its subsequent effects. Trauma is an emotional response to a distressing event. This could be an accident, war, abuse, neglect, or extreme fear. It isn’t uncommon for the emotional shock to last long after the immediate threat has subsided, disrupting daily life dramatically. Far from a short-lived, distressing experience, trauma can persist indefinitely, impacting both mental and physical health.
Additionally, the response to trauma can vary, forming distinct patterns in behavior. For example, some individuals may experience intense anxiety, panic attacks, depression, or suicidal ideation. In others, trauma can cause disassociation, an element that contributes significantly to detachment from reality.
On the physiological level, trauma can trigger the body’s stress response, resulting in physiological changes like increased heart rate, rapid breathing, and heightened alertness. Long-term trauma exposure can lead to chronic disorders such as Post-Traumatic Stress Disorder (PTSD) or Complex PTSD.
In the context of alcohol use disorder, trauma has a considerable influence. Often, suffering individuals turn to alcohol as a means to cope with their traumatic experiences. This habit can quickly escalate into dependence, leading to alcohol use disorder. Therefore, an effective alcohol use disorder treatment plan must take into consideration the underlying trauma, addressing both issues simultaneously for holistic healing.
The Link Between Trauma and Alcohol Use Disorder
Continuing from the previous section, let’s delve deeper into the connection between trauma and alcohol use disorder, examining the triggers and biological factors that come into play.
Self-Medication Hypothesis
Numerous studies point towards the Self-Medication Hypothesis, proposing that individuals with traumatic experiences often self-medicate with alcohol. It’s a way to numb emotional pain and distract themselves from disturbing memories.
However, this temporary solace may lead to a relentless cycle of dependency, transforming into an alcohol use disorder over time. For instance, consider a population suffering from PTSD—Post Traumatic Stress Disorder—statistics reveal disturbing numbers where about 20% of them turn towards alcohol, indicating a dire need for integrated alcohol use disorder treatment protocols.
Neurobiological Factors
Further, specific biological factors merit attention. Research indicates potential changes in the part of the brain termed the ‘Hypothalamic-Pituitary-Adrenal’ axis, igniting a heightened stress response in trauma victims. This heightened state, coupled with increased axiolytic effects of alcohol, makes alcohol increasingly appealing, strengthening the alcohol-trauma connection. In essence, trauma appears to trigger brain alterations that make the affected more susceptible to alcohol use disorder, highlighting the necessity for precision treatment plans.
Addressing Trauma in Alcohol Use Disorder Treatment
Understanding the relationship between trauma and alcohol use disorder paves the way for effective treatment. Tailoring alcohol use disorder treatment plans, incorporating trauma-specific therapies, plays an essential role in recovery.
Importance of Incorporating Trauma Therapy in Treatment
Recognizing trauma as an underlying cause of alcohol use disorder, its integration into treatment plans promotes recovery. Trauma-focused Cognitive Behavioral Therapy (TF-CBT), Eye Movement Desensitization and Reprocessing (EMDR), and Somatic Experiencing allow individuals to address traumatic experiences instead of resorting to alcohol as a coping mechanism.
The Role of Personalized Treatment Plan in Recovery
Bespoke treatment plans, addressing both trauma and alcohol use, afford individuals the best chance at recovery. With this approach, I design a comprehensive plan that includes medication management, psychotherapy, and holistic practices like meditation and yoga. This bespoke treatment caters to the needs of an individual, ensuring mental and physical wellbeing are prioritized.
The Place of Medical Detox in Alcohol Use Disorder Treatment
Detoxification remains a key aspect of alcohol use disorder treatment. Medical detox assists in managing withdrawal symptoms, providing a safer environment for recovery. It’s crucial to note that detox alone can’t address the roots of the addiction – trauma. Hence, it’s advisable to follow detox with a comprehensive treatment plan addressing alcohol dependence and the underlying trauma.
Incorporating Aftercare in Alcohol Use Disorder Treatment
The recovery journey extends beyond the initial treatment. Aftercare, including ongoing therapy, support groups and relapse prevention training, reinforces the tools acquired in treatment. This continuous support facilitates a life of sobriety, enhancing resilience to stress and helping individuals to cope without the crutch of alcohol.
Supportive Interventions
Building on the prior link between trauma and alcohol use disorder, I’ll delve into the role of supportive interventions. Evidence suggests that implementing trauma-informed care in alcohol use disorder treatment can aid in recovery. With treatments tailored to each individual’s unique experiences and symptoms, they address both the alcohol use disorder and underlying trauma.
Customized Treatment Plans
Personalized treatment plans form the crux of effective recovery. Incorporating medication management, psychotherapy, and holistic practices, these plans aim to address the unique needs and symptoms of each individual.

For instance, trauma-focused Cognitive Behavioral Therapy (TF-CBT) assists in tackling distressing thoughts and emotions linked to trauma, while Eye Movement Desensitization and Reprocessing (EMDR) aids in processing traumatic memories. Traditional detoxification can’t be overlooked, as managing withdrawal symptoms forms an integral part of recovery.
Life Skills Training
Developing life skills such as stress management, resilience, problem-solving, and communication aids in achieving long-term sobriety. Hence, many alcohol use disorder treatment plans include life-skills training. These abilities allow individuals to manage triggers and stresses without resorting to alcohol, fostering greater resilience and effectiveness in daily life.
Aftercare Programs
Aftercare isn’t merely about preventing relapse; it’s about equipping individuals with the tools to navigate life sober. Regular therapy sessions, support groups, and relapse-prevention training form the backbone of most aftercare programs. They contribute to maintaining long-term sobriety and enhancing resilience to stress without the need for alcohol.
Altogether, supportive interventions can improve outcomes for individuals grappling with both trauma and alcohol use disorder. By addressing the two concurrently, treatment plans can foster a more robust and sustained recovery.
Importance of Early Intervention
The interplay between trauma and alcohol use disorder isn’t just a correlation—it’s a complex relationship that requires comprehensive, individualized treatment strategies. It’s essential to recognize that trauma often serves as a catalyst for alcohol use disorder. It’s not just about treating the addiction, but also addressing the underlying trauma.
Incorporating trauma-specific therapies into treatment plan has proven effective. Personalized treatment, including medication management and holistic practices, can pave the way for recovery. Supportive interventions, like life skills training and aftercare programs, are equally critical.
Let’s remember, early intervention can make all the difference. It can halt the progression from trauma to alcohol dependency, and promote resilience to stress without the need for alcohol. So, let’s not wait. Let’s address trauma and alcohol use disorder together, and empower individuals to reclaim their lives.


 How to Maximize Your Rehab Insurance Benefits
How to Maximize Your Rehab Insurance Benefits  Everything You Need to Know About Car Transport for a Big Move
Everything You Need to Know About Car Transport for a Big Move  Why DUI Accidents Demand The Expertise Of A Lawyer
Why DUI Accidents Demand The Expertise Of A Lawyer 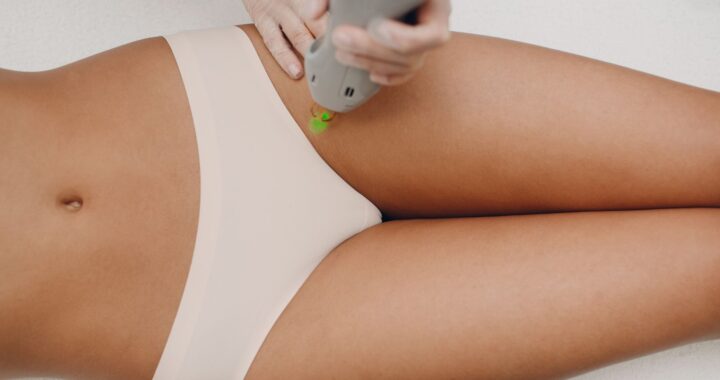 Bikini Underwear: Finding the Perfect Fit for All-Day Comfort
Bikini Underwear: Finding the Perfect Fit for All-Day Comfort  How to Satisfy Your Taco Cravings in Minutes by Ordering Tacos Online
How to Satisfy Your Taco Cravings in Minutes by Ordering Tacos Online  Finding a Luxury Resort in Belize
Finding a Luxury Resort in Belize